Diabetes is a chronic, incurable disease that occurs when the body doesn’t produce any or enough insulin, leading to an excess of sugar in the blood.
Insulin is a hormone produced by the pancreas. It can be thought of as a key to unlock the doors of sugar channels in the body which help sugar (glucose) to move from the blood into the cells. This is how the body controls blood glucose.
If you have diabetes, the glucose in your blood cannot pass into your cells to be used or stored as energy, causing high blood glucose (hyperglycemia).
Difference between Type 1 and Type 2 diabetes?
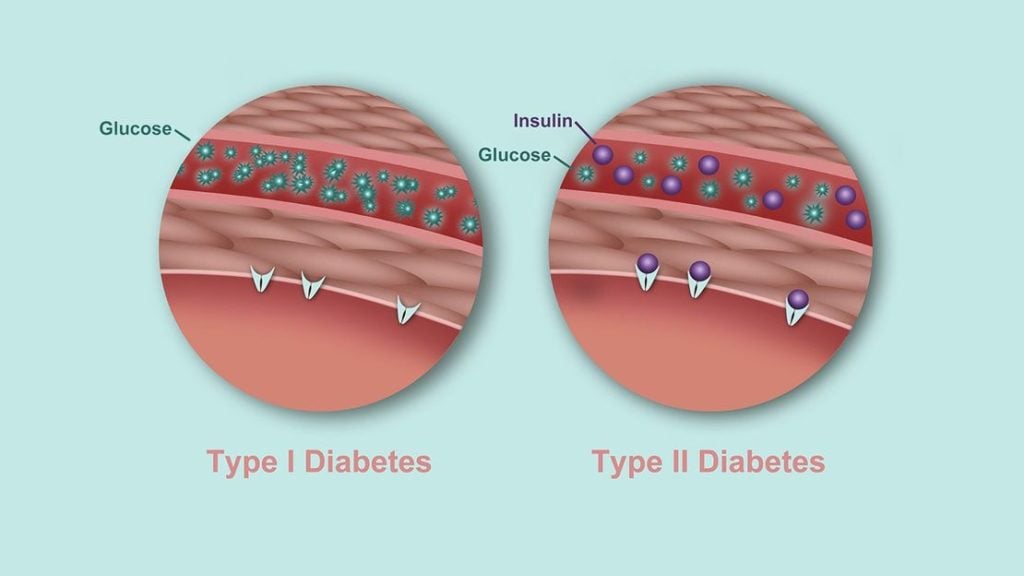
When you have Type 1 diabetes, insulin is not produced by the body.
· Exogenous insulin (insulin injected from the outside) will be needed to help open the door to allow glucose to enter cells.
When you have Type 2 diabetes, insulin is created by the body but the body does not respond well to it. This is also known as insulin resistance.
· Lifestyle changes, medication and possibly injected insulin will be needed to help glucose enter the cell.
Neither type is better or worse; they are just different in how they arise and their management.
What are the main causes of type 2 diabetes?
– Lack of physical activity
– High blood pressure (Hypertension)
– High cholesterol
– History of gestational diabetes
– History of pre-diabetes
– Overweight
– Genetics
However, unlike type 1 diabetes, type 2 diabetes can be prevented or even reversed with healthy eating, physical activity, and medication!
Reference:
About Diabetes. (2017). Canadian Diabetes Association. Retrieved 13 May 2017, from https://www.diabetes.ca/about-diabetes
How do I manage my diabetes?
After a diabetes diagnosis, it can be overwhelming. Many people feel like they have to start avoiding certain foods and the most common question I get is “Should I still eat this? Can I still have that?”
The truth is, there’s no special diet for people with diabetes, and it is essentially the same diet as for people without diabetes. But, with that said, if your usual diet vastly differs from the general recommendation, then you will definitely benefit from making better food choices. Additionally, it would be ideal to compliment it with physical activity and medication if prescribed by your doctor.
FOOD
We are all foodies to some extent, and I want to assure you firstly that you still have the flexibility to create your own dishes and meal plans. The healthy eating recommendations are still the same as before your diagnosis. However, it is essential to know how different food may affect your blood sugar. It depends on:
1) the type of food you eat
2) how much you eat and,
3) the combination of food types you eat
Learn about carbs counting
- For people with type 1 diabetes, and those with type 2 diabetes who require insulin, carbohydrate counting is a way of matching insulin requirements with the amount of carbohydrate that you eat or drink.
- For people with type 2 diabetes who do not require insulin, carbohydrate counting is a way to regulate the amount of carbohydrate you consume. This can monitor how this may affect your blood glucose control, weight management and medication intake.
The reason we have to count carbohydrates is because carbohydrate often has the biggest impact on our blood sugar levels. However, we should never avoid carbohydrates either because your body depends on them to function properly.
Learn about portion sizes
When you learn how to carb count, you immediately learn about the portion sizes. Find out what portion size is appropriate for each type of food.
As the saying goes “Keeping your serving sizes in check, as that can help keep complications from diabetes at bay.”
Make every meal well-balanced
We understand it can be difficult, but try to include starches, fruits, vegetables, protein and fats in every meal.
As mentioned earlier, carbohydrate is the main food group that causes your blood sugar level to rise, while protein does not significantly impact your blood sugar.
Therefore, eating too much carbohydrates that are quickly digested can result a spike in your blood sugar. However, when you pair it with protein, it slows down the digestion of carbohydrates, which prevent blood sugar spikes.
Finally, limit sugary beverages. They are loaded with sugar, which would lead to a sharp raise in your blood sugar.
PHYSICAL ACTIVITY
Consider brisk walking for 30 minutes 5 times per week, or 1 hour 3 times a week. It can also be other forms of enjoyable physical activity.
Start slow, and gradually increase your activity.
Try parking further away from the shops, getting off a few bus stop early or taking the stairs. These can all count towards your physical activity everyday.
MEDICATION
Your doctor may prescribe medications to compliment your lifestyle changes. Take them regularly! Setting an alarm on your phone or having them with you on-the-go can help increase compliance. If you have problems with your medication, discuss treatment choices with your doctor.
Aim for your A1c to be less than 7%, or a target agreed with your doctor. Make sure you have decided on a screening schedule with your doctor to avoid and prevent irreversible complications.
Last but not least…
All these information can be overwhelming. Talk to your doctor, nurse or dietitian about the best food choices, physical activity and medication. Remember, no one diet is the best for everyone. Talk to your health care team to find a lifestyle that fits you!
Don’t forget, you can have a perfectly normal life free of complications by controlling your diabetes well!
Reference:
About Diabetes. (2017). Canadian Diabetes Association. Retrieved 13 May 2017, from https://www.diabetes.ca/about-diabetes


